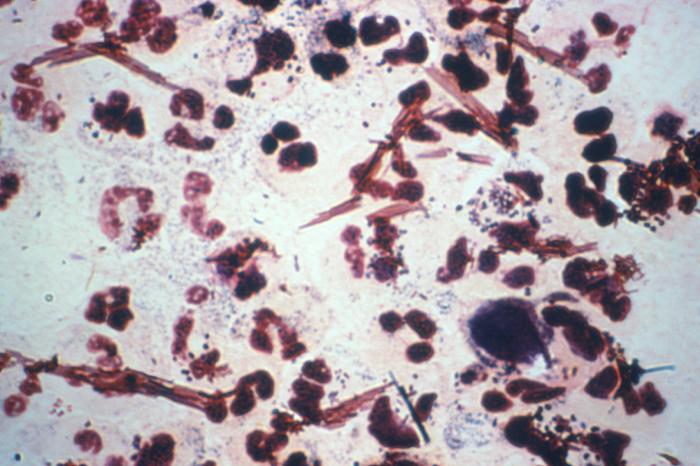
Neisseria gonorrhoeaeOverview: Neisseria gonorrhoeae is a Gram-negative, aerobic, non-motile, non-spore-forming diplococcus bacterium and a member of the family Neisseriaceae of the β subclass of the class Proteobacteria (Figure 1). The organism is oval or bean-shaped, roughly 0.6 μm (micrometres) to 1.0 μm in diameter, and is typically observed in pairs with its long side parallel. N. gonorrhoeae is also strongly oxidase-positive, is optimally grown at 35°C to 36°C on Thayer-Martin agar and other media that contain 10% carbon dioxide (suggesting the species is capnophilic), and it only oxidizes glucose (Figure 2). This pathogen also possesses fimbriae (pili) that extends several micrometers (μm) from its surface and operates mechanistically similar to a grappling hook, allowing the bacteria to adhere to surfaces. They are fragile and fastidious, dying on drying, die rapidly in the environment, and the only known host is mankind. Figure 1. This poorly colorized Gram-stain image of a urethral discharge specimen reveals the presence of Neisseria gonorrhoeae bacteria.
Figure 2. These were two culture plates used to grow colonies of Neisseria gonorrhoeae bacteria. Known as “overgrowth”, note that the “non-selective” chocolate agar medium on the right, due to its composition, allowed for the growth of organismal colonies other than those of Neisseria gonorrhea, while the “selective” Thayer-Martin medium on the right, containing antimicrobials that inhibit the growth of organisms other than N. gonorrhoeae, shows no overgrowth, but is positive for N. gonorrhoeae. Virulence and Pathogenicity: There are four different types of strains of this species, namely, T1, T2, T3, T4, and are classified by their fimbriae. Its outer membrane is composed of proteins, phospholipids, and lipopolysaccharides (LPS). The lipopolysaccharides of N. gonorrhoeae are different than those found in enteric bacteria because they are highly-branched basal oligosaccharides and do not possess the repeating O-antigen subunits. Hence, Neisserial LPS is referred to as lipooligosaccharide (LOS). During their growth, the outer membrane releases fragments known as “blebs,” and it is these blebs that contain the LOS which are thought to have a role in pathogenesis during their infection process. N. gonorrhoeae cell walls contain proteins that reside on the outer membrane surface or span the outer membrane (integral proteins). There are several different types of gonococcal outer membrane proteins and each imparts a different biological role during infection, including the elicitation of humoral and cell-mediated immune responses, decreased leuocyte association, and resistance to bactericidal effects of normal human serum. There are three main types of outer membrane proteins found in N. gonorrhoeae, namely, porins or protein I (denoted Por), outer membrane opacity proteins (denoted Opa), and reduction modifiable protein (denote Rmp). Generally, each strain of the bacteria expresses only one type of this protein, but there are different variations associated with this protein and it is these variations that account for the different antigenic types of the organism. Por proteins (PorA and PorB) are heat-stable integral proteins and function as anion-specific channels through the pathogen's outer membrane. Por proteins may function in cell-cell interaction by collapsing the membrane potential on contact with epithelial cells and may influence intracellular killing of organisms in polymorphonuclear leukocytes by preventing phagosome-lysosome fusion and diminishing oxidative burst. The Opa proteins are usually found on colonies that have an opaque phenotype known as 0+, and there may be none, one, or many expressed on the outer surface of the bacterium. Opa proteins augment pilus-mediated adherence to mucosal surfaces and also facilitate mucosal cell invasion. These proteins are heat-labile and typically have a molecular weight of approximately 24 to 28 kiloDaltons. Interestingly, Opa proteins are influenced by the menstrual cycle. Finally, Rmp is found on every strain of the bacterium and is complexed with Por and LOS, but does not undergo antigenic variation like the other proteins (Winn et al., 2006). The bacteria use these outer membrane proteins and their fimbriae to invade the host. First the bacteria use their fimbriae to attach to non-ciliated epithelial cells of the fallopian tube, and then they enter the epithelial cells by parasite-directed endocytosis. Throughout the endocytosis process, the membrane of the cell pulls in and pinches off a membrane bound vacuole that has the bacteria inside of it. This vacuole travels to the base of the cell so that the bacteria can be released into the subepithelial tissue, and now can successfully cause infection in the host. Once successfully inside the host, the bacterium produces two types of extracellular IgA proteases that have the ability to cleave different areas of the hinge region of heavy chain human immunoglobulin molecules. Cell damage is caused by the release of LOS and peptidoglycan, which activate the alternative complement pathway and the production of tumor necrosis factor. Clinical Infections: N. gonorrhoeae is responsible for causing the venereal disease gonorrhea. It infects organs alternately: urethra nor vagina, cervix not uterus, fallopian tube not the fimbriae of uterine tube, ovary not posterior abdominal wall. Salpingitis (fallopian tube infection) leads to tubal blockage and pelvic inflammatory disease. Urethritis, prostatitis, and epididymo-orchitis are the common infections in males. Rectum and pharynx are infected by direct contact with infectious discharge, usually urethral, causing proctitis (Spicer, 2008). Everyone that is sexually
active is at risk for contracting this disease,
as well as newborns through the birth canal of
an Signs and Symptoms: Some men with gonorrhea may have no symptoms at all. However, some men have signs or symptoms that appear two to five days after infection; symptoms can take as long as 30 days to appear. Symptoms and signs include a burning sensation when urinating, or a white, yellow, or green discharge from the penis. Sometimes men with gonorrhea get painful or swollen testicles. In women, the symptoms of gonorrhea are often mild, but most women who are infected have no symptoms. Even when a woman has symptoms, they can be so non-specific as to be mistaken for a bladder or vaginal infection. The initial symptoms and signs in women include a painful or burning sensation when urinating, increased vaginal discharge, or vaginal bleeding between periods. Women with gonorrhea are at risk of developing serious complications from the infection, regardless of the presence or severity of symptoms. Symptoms of rectal infection in both men and women may include discharge, anal itching, soreness, bleeding, or painful bowel movements. Rectal infection also may cause no symptoms. Infections in the throat may cause a sore throat but usually causes no symptoms. Although this bacterium does not have a high mortality rate, it has a high prevalence rate, which is why it is very important to educate people about sex, get tested often for sexually transmitted diseases, and if possible, not have sex until marriage. Reference: Spicer, J. (2008). Clinical Microbiology and Infectious Diseases (2nd ed.). Churchill Livingstone. Winn, W., Allen, S., Janda, W. et al. (2006). Koneman's Colar Atlas and Textbook of Diagnostic Microbiology (6th ed.). Baltimore: Lippincott Williams & Wilkins. |
Diplococcal: A diplococcus (plural diplococci) is a round bacterium (a coccus) that typically occurs in pairs of two joined cells (shown below).

Asymptomatic: In medicine, a disease is considered asymptomatic if a patient is a carrier for a disease or infection but experiences no symptoms. A condition might be asymptomatic if it fails to show the noticeable symptoms with which it is usually associated. Asymptomatic infections are also called subclinical infections. The term 'clinically silent' is also used.
|