ShigellaOverview: Shigella
is a genus of bacteria belonging to the family
Enterobacteriaceae. Species of this genus are Gram-negative,
rod-shaped, and non-lactose
fermenting (with exception to S. sonnei). They are also
non-motile due to the lack of flagella and makes
ATP (an energy molecule) by aerobic respiration
if oxygen is present, but is also capable of
switching to fermentation - facultative
anaerobe. Shigella species can ferment
carbohydrates with the production of acid, and grow in translucent
white colonies (Figure 1). Shigella are closely
related to Escherichia coli and Salmonella and share common antigens with one
another and other enteric
bacteria. There are four species of Shigella:
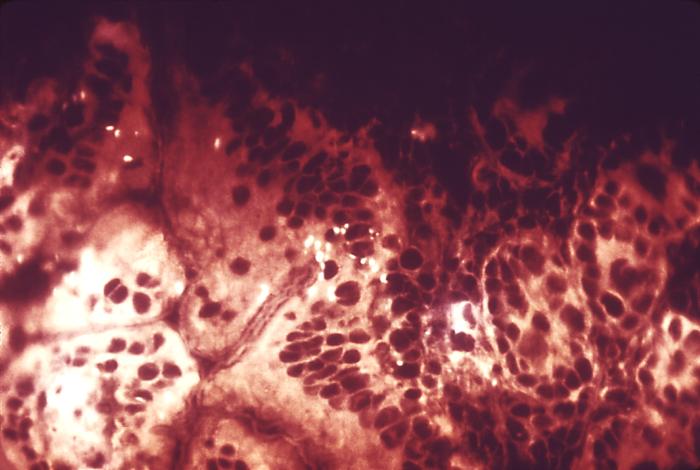
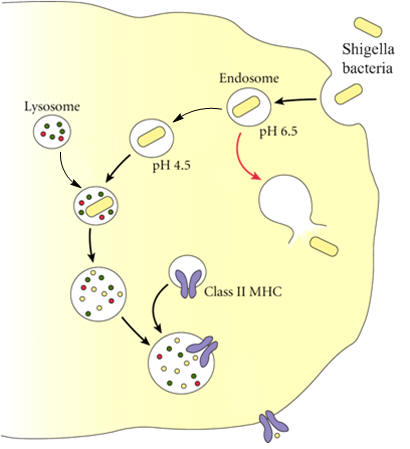
S. boydii, S. dysenteriae, S. flexneri, Figure 1. This photograph depicts the colonial morphology displayed by Shigella boydii bacteria cultivated on a Hektoen enteric agar surface. Symptoms and Disease: Shigella causes Shigellosis, an infectious disease that causes watery loose stool, diarrhea, vomiting, stomach cramps, and high fever (Figure 2). The infection lasts five to seven days, but children, the elderly, and individuals who are immunosuppressed are more prone to severe cases of shigellosis. In fact, if left untreated, the diarrhea can cause death, and seizures can result due to high fever. S. sonnei causes the most cases of Shigellosis. Figure 2. This micrograph reveals 2nd stage shigellosis progression; the Shigella bacteria have penetrated the intestinal mucosa Symptoms can take about a week to
manifest itself, and the bacteria
stays in the host for about a week or two after
the illness has surpassed, and
thus is still transferable. It is transmitted
from person-to-person, most often due to
unhygienic practices, and is common in
developing countries where Prevalence: S. flexneri is responsible for 60% of the disease in developing countries, S. sonnei causes 77% of cases in developed countries and 15% in developing countries, and S. dysenteriae usually causes epidemics of bloody diarrhea, most often in confined populations (El-Gendy et al., 1999). Shigellosis is spread by fecal-oral contamination, and primates are the hosts. The Shigella toxin affects the small intestine, causing a transduction of fluid into the intestinal lumen and subsequent diarrhea. The diarrhea causes destruction of the epithelial cells of the intestinal mucosa. Immune Evasion and Infection: Some strains of Shigella produce enterotoxins. An enterotoxin (not to be confused with endotoxin: a toxin that is released from certain bacteria as they disintegrate in the body) is a protein toxin released by a microorganism in the intestine. One such example is the enterotoxin Shiga toxin, which causes hemolytic uremic syndrome (bloody diarrhea) or Reiter's disease after shigellosis. The Shiga toxin acts on the lining of the blood vessels, the vascular endothelium. It is made up of an A-subunit (toxic) and a B-subunit. The B-subunit of the toxin binds to a component of the cell membrane known as Gb3 and the complex is engulfed by the target cell. When the protein is inside the cell, the A-subunit interacts with the ribosomes to inactivate them (See diagram). The A-subunit of Shiga toxin is an N-glycosidase that modifies the RNA component of the ribosome to inactivate it and so brings protein synthesis to a halt, leading to the death of the cell. The vascular endothelium has to continually renew itself, so this killing of cells leads to a breakdown of the lining and to hemorrhage. The first response is commonly a bloody diarrhea. This is because Shiga toxin is usually taken in with contaminated food or water. Shigella species have a large virulence plasmid that carries the genes necessary for invasion and colonization of the epithelial cell layer of the human gut resulting in dysentery (bloody diarrhea) (Dorman, 2009). Shigella moves around from cell to cell by using proteins (IcsA) that trigger actin polymerization in the host cell in a "rocket" propulsion fashion (Taylor, 2008). In fact, in order to evade the host's immune system, Shigella species avoid being presented by MHC class II molecules by escaping from the endosome/phagosome (both terms are synonymous) after being engulfed, before it fuses with a lysosome containing enzymes that digest the bacteria and prevent it from causing harm (Figure 3). Figure 3. Immune evasion strategies used by Shigella species to prevent being presented by MHC Class II molecules. Identification: In order to diagnose diseases caused by Shigella, laboratory tests must be performed by rectal or fecal swab tests. These tests can help determine the strain of the bacteria that is causing the infection, so appropriate antibiotics can be prescribed. Once the symptoms of the disease are noted, it is determined that the pathogen causing the infection is Shigella if tests show up negative for motility, Gram staining and Urea Hydrolysis, no gas production from carbohydrates, have translucent white colonies on MacConkey agar (Figure 1), and are usually biologically inert (El-Gendy et al., 1999). Indole reactions are sometimes positive and sometimes negative, with the exception of S. sonnei which is always negative. Shigella usually become resistant to antibiotics
quickly, and so antibiotics are
prescribed when absolutely necessary, especially
in cases of epidemics. Once
infected, the person is not likely to get
infected by that same strain for a while,
but is still at risk of getting infected by
other strains of Shigella. Due to the References: Bhardwaj, G., & Panhotra, B.R. (1985). Which chemotherapy for Shigella dysentery? Indian Journal of Pediatrics, 52(5): 451-452. Dorman, C. (2009). The Virulence Plasmids of Shigella flexneri. Microbiology Monographs, 11: 151-170. El-Gendy, A., El-Ghorab, N., Lane, E.M., Elyazeed, R.A., et al. (1999). Identification of Shigella flexneri Subserotype 1c in Rural Egypt. Journal of Clinical Microbiology, 37(3): 873–874. Taylor, M.C. (2008). Enterohaemorrhagic Escherichia coli and Shigella dysenteriae type 1-induced haemolytic uraemic syndrome. Pediatric Nephrology, 23(9): 1425-1431. |