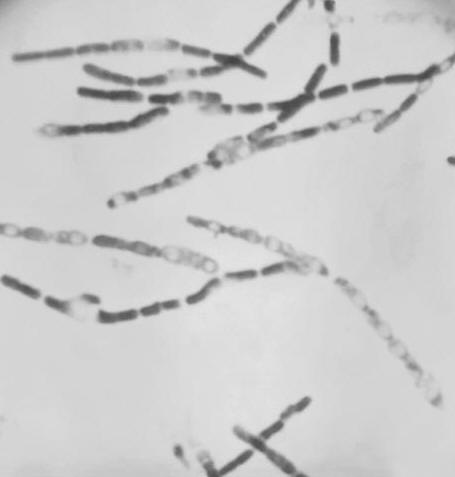
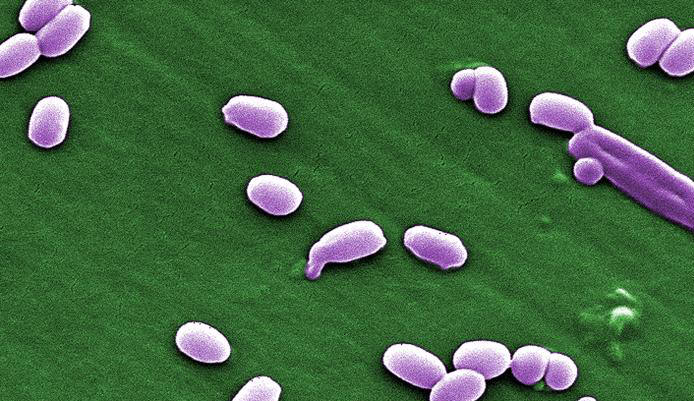
Bacillus anthracisOverview: Bacillus anthracis is a relatively large Gram-positive, rod-shaped bacterium, found throughout the world in a wide range of environments and in a wide variety of large mammalian hosts. This organism is roughly 3 to 5 μm (micrometres) by 1.2 μm in size, and organizes its colonies into long chains (Figure 1). It is endospore-forming and requires oxygen as a terminal electron acceptor to maintain its normal aerobic metabolism (Figure 2). Moreover, B. anthracis is catalase-positive, suggesting that this organism is able to chemically breakdown hydrogen peroxide into water and oxygen. This pathogen also tests positive for the lecithinase, indicating that it has the ability to degrade lecithin - a cell membrane component abundant in nerve tissue and egg yolk. In contrast, not all Bacillus species test positive for lecithinase. Some key characteristics that distinguish B. anthracis from the common Bacillus species are indicated in Table 1. Figure 1. This photomicrograph depicts a number of Gram-positive, endospore-forming Bacillus anthracis bacteria. Figure 2. This scanning electron micrograph depicts spores produced by Bacillus anthracis bacteria. A key characteristic of B. anthracis is the smooth surface of the protein coat of these bacterial spores. These spores can live for many years which, enables the bacteria to survive in a dormant state. Table 1. A comparison between Bacillus anthracis and the common Bacillus species.
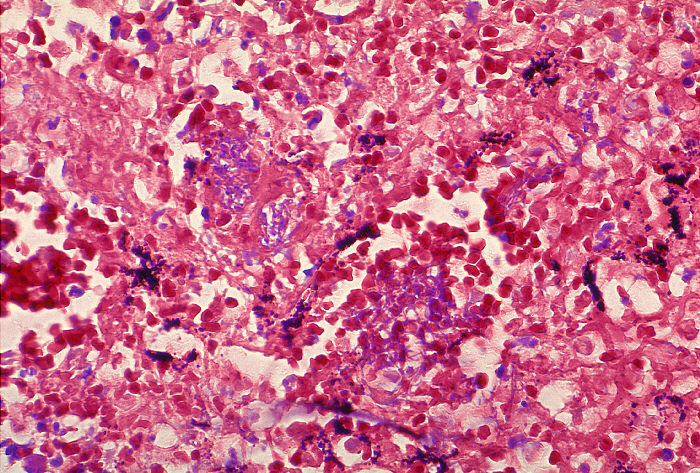
Infection and Disease: This pathogen has the ability to cause disease in humans and its virulence stems from its ability to form endospores which produce three major virulence factors, namely: edema toxin, lethal toxin, and a capsular polysaccharide (Pier et al., 2004). The spores formed by B. anthracis commonly remain dormant; however, if they enter the body, they will germinate and become pathogenic. This causes the disease known as Anthrax. These endospores exist in their dormant form, found in soil, animal feces, and carcasses of sheep, goats, cattle, bison, horses and deer. The spores infect humans in three ways, namely, through broken skin (cutaneous anthrax), oral ingestion (gastrointestinal anthrax), and inhalation (inhalation anthrax). As with other pathogenic bacteria, B. anthracis must acquire iron in order to grow and proliferate in its host environment. The most readily available iron sources for pathogenic bacteria are the heme groups used by the host in the transport of oxygen. In order to scavenge heme from host hemoglobin and myoglobin, B. anthracis uses two secretory siderophore proteins, IsdX1 and IsdX2. These proteins can separate heme from hemoglobin, allowing surface proteins of B. anthracis to transport it into the cell Anthrax infection through the skin has a relatively low mortality rate and can often go away without treatment. On the contrary, infection through ingestion of meat from infected animals can be fatal. Although treatable, it is difficult to diagnose and has mortality rate of 20 to 60%. The bacteria in this case invades the intestinal walls and spreads via the bloodstream. When anthrax endospores are inhaled and absorbed into the bloodstream, they migrate to lymph glands in the chest where they will proliferate, spread, and produce toxins leading to fatal results (Figure 3). Figure 3. Histopathology of mediastinal lymph node in fatal human anthrax using Giemsa stain. Immunity and Vaccination: Anthrax disease equally affects humans, regardless of one's age, race or sex. Natural occurrences of this disease in the United States, Canada, and Europe are uncommon, but risks are found among veterinarians, farmers, and individuals who handle animal wool, hair, hides, or bone products. This disease is more commonly found throughout Africa and parts of Asia, where it is used in bioterrorism / warfare. For control and immunity to anthrax, a vaccine is available against a component common to both the edema and lethal toxins. This vaccine, however, is mainly issued to military personnel along with those at high risk that handle anthrax in a laboratory setting. Also, those who are at risk from the occupations mentioned above are recommended to take the vaccine. Current injectable anthrax vaccines work primarily by eliciting antibody to protective antigen. The capsule is made up of poly-D-glutamic acid; as such, the D-glutamic acid polymer is not terribly immunogenic due to the inability of antigen-presenting cells to degrade the D form of the amino acid polymer chain (Pier et al., 2004). Finally, anthrax is not a contagious disease. It should be noted, however, that there have been cases where anthrax was contracted through open sores coming into contact with lesions from infected individuals. References: Pier, G.B., Lyczak, J.B., & Wetzler, L.M. (2004). Immunology, Infection, and Immunity. Washington: ASM Press. |