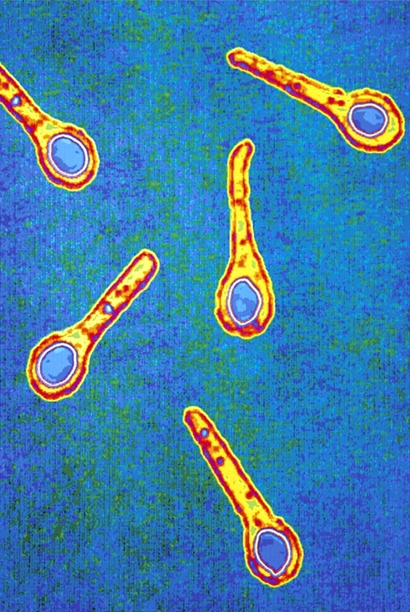
Clostridium botulinumOverview: Clostridium tetani is a Gram-positive, spore-forming, rod-shaped bacterium that is resistant to temperature modifications, moisture, and chemical disinfectants. C. tetani is strictly anaerobic and dies in the presence of oxygen; however, spores produced by this species are able to withstand oxygenated environments and other harmful environments. The endospores are produced in a swollen sporangium and their shape generally resembles a 'drumstick' (Figure 1). Under anaerobic conditions, C. tetani spores geminate and produce exotoxins, namely, tetanospasmin (tetanus neurotoxin, abbreviated TeNT) and tetanolysin. The genes encoding these toxins are located on separate plasmids within the bacterium. Figure 1. Clostridium tetani endospores in a swollen sporangium. Virulence and Pathogenicity: Tetanus toxin is the neurotoxin produced by the vegetative cell of C. tetani when spores germinate under anaerobic conditions in an open wound, causing tetanus. The toxin has no known function for clostridia (sulfite-reducing bacteria) in the soil environment where they are normally encountered. Tetanus toxin spreads through tissue spaces into the lymphatic and vascular systems. It enters the nervous system at the neuromuscular junctions and migrates through nerve trunks and into the central nervous system by retrograde axonal transport. The protein tetanus toxin has a molecular weight of 150 kDa (kiloDaltons). It is made up of two parts, namely, a 100 kDa heavy or B-chain and a 50 kDa light or A-chain. The chains are connected by a disulfide bond. The B-chain binds to cell surface disialogangliosides (GD2 and GD1b) on the neuronal membrane. The A-chain, a zinc-based endopeptidase, attacks the vesicle-associated membrane protein. The action of the A-chain stops the affected neurons from releasing the inhibitory neurotransmitters GABA (gamma aminobutyric acid) and glycine by degrading the protein synaptobrevin, a small integral protein of secretory vesicles. This results in a failure to inhibit motor reflexes from the smallest stimulus, which causes life-threatening muscle spasms, termed a tetanic spasm. Similarly, neonatal tetanus occurs in infants born without protective passive immunity, because the mother is not immune. It usually occurs through infection of the unhealed umbilical stump, particularly when the stump is cut with an unsterile instrument (Figure 2).
Figure 2. This neonate is displaying a bodily rigidity produced by Clostridium tetani exotoxin, called neonatal tetanus. Tetanolysin directs the multiplication of the bacteria, which is also associated with tetanus (Atriham and Crown, 2007). The exotoxin belongs to a family of protein toxins known as cytolysins which bind to cholesterol. Cytolysins form pores in the cytoplasmic membrane that allows for the passage of ions and other molecules into the cell. The molecular weight of tetanolysin is approximately 55 kDA. Diagnosis: Diagnosis of C. tetani is based on clinical features rather than laboratory verification. Most tetanus infections are results of small punctures to the skin that become infected with C. tetani spores. Some of the symptoms of tetanus include hypertonia and generalized muscle spasms, in absence of other noticeable medical causes.
Figure 3. Sir Charles Bell's portrait of a soldier dying of tetanus. The characteristic rigidity of the body is referred to as opisthotonos and risus sardonicus. Risk Factors:
Race, sex, and age have some associations with
tetanus. In fact, the highest incidence of tetanus was
found in Hispanics, followed by whites and then
African Americans. Also, men are believed to be better protected
against tetanus than women, due to additional
vaccination for reasons such as military and
professional needs. Finally, the incidence of
tetanus increases as people age. C. tetani spores can be found in soil, dust, animal intestines and human feces. Generally, humans are not carriers of this pathogen; thus, carrier rates are low and range between 0 and 25%. Likewise, this organism is not a regular member of the human intestinal flora and only passes through depending on ingestion. Immunity and Vaccination: Treatment of tetanus includes treating wounds and managing the pain caused by the symptoms and complications due to tetanus. Anti-tetanus immunoglobulin and antibiotics should be given immediately and may be beneficial in stopping progression of the infection. Contracting the tetanus disease does not cause immunity. The amount of the tetanus toxin is not high enough to induce an immune response to it; therefore, vaccinations for tetanus are required. Administration of inactivated tetanus toxin, also known as a toxoid, induces antibody responses in hosts and stops C. tetani from causing tetanus (Casadevall and Pirofski, 1999). Injections of tetanus toxoid are given at various stages throughout life. Three injections are given to babies in their first year; a booster is given one year later and another booster is given when children begin school. Even if immunized, people who sustain a dangerous wound should be given a tetanus toxoid injection. References: Atriham, A., & Crown, L.A. (2007). Tetanus: Uncommon, But Still a Threat. American Journal of Clinical Medicine, 4(1): 3-5. Casadevall, A., & Pirofski, L. (1999). Host-Pathogen Interactions: Redefining the Basic Concepts of Virulence and Pathogenicity. Infection and Immunity, 67(8): 3701-3713. |
Retrograde axonal transport: The transport of vesicles from the synaptic region of an axon towards the cell body.
|