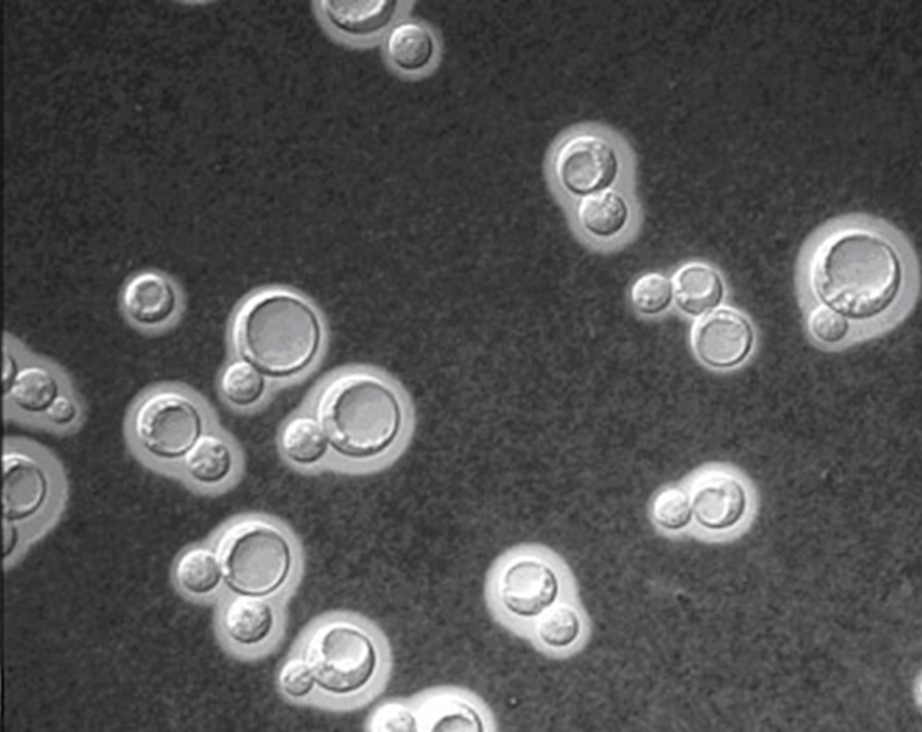
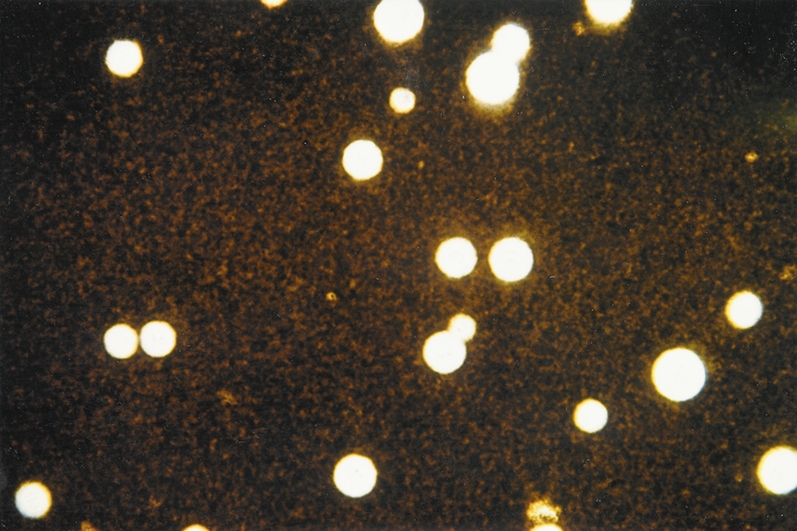
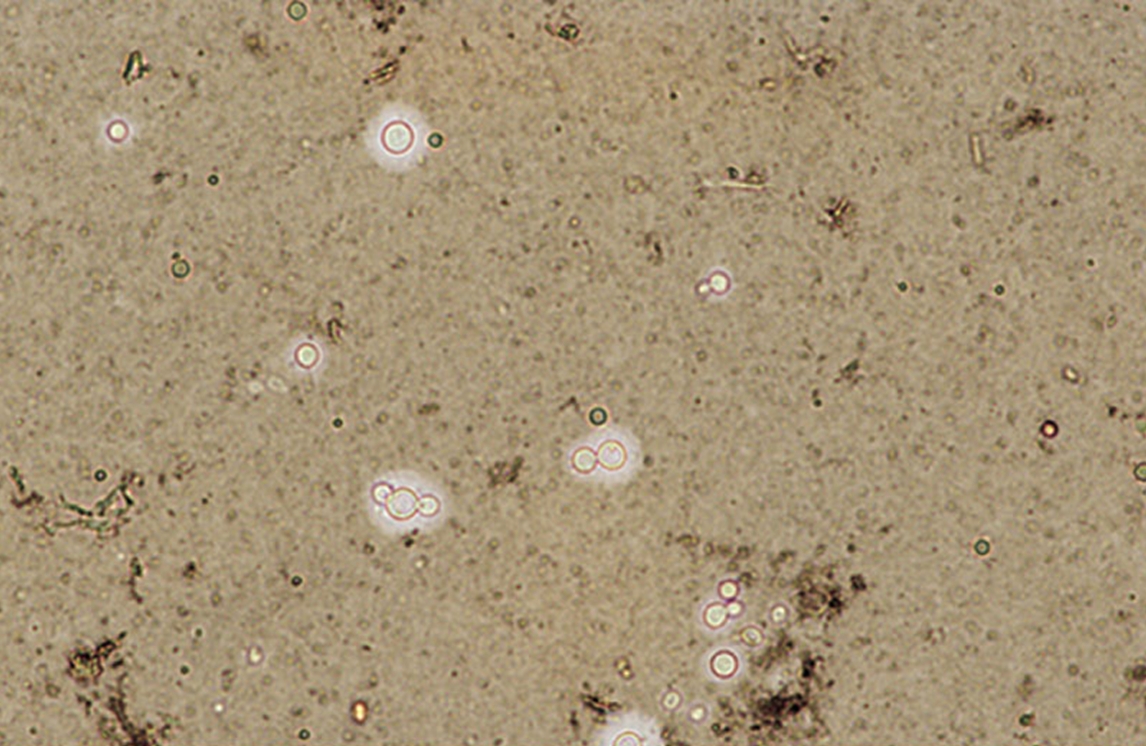
Cryptococcus neoformansOverview: Cryptococcus neoformans is an unicellular, encapsulated, non-motile, non-spore-forming, non-lactose fermenting, anaerobic yeast-like fungus that possesses a thick polysaccharide cell wall and causes the infection cryptococcosis (Figure 1). The organism is coccus-shaped and roughly 6 μm (micrometres) to 8 μm in diameter. C. neoformans is commonly found in pigeon (Columba livia) droppings found in the United States and other temperate climates. However, the species has the ability to survive and grow in both plants and animals. Colonies of C. neoformans are fast growing and appear soft, glistening to dull, and cream or yellowish brown in colour. The species is closely related to Candida albicans, except that Candida is known to form well-developed pseudohyphae, whereas C. neoformans fungi do not. C. neoformans is composed of two varieties (v.): C. neoformans v. neoformans and v. grubii. A third variety, C. neoformans v. gattii, is now considered a distinct species, Cryptococcus gattii. Figure 1. Cryptococcus neoformans yeast cells. Identification: C. neoformans capsule is composed of a backbone of mannose substituted with xylose and glucuronic acid, referred to as glucuronoxylomannan, much like many bacterial pathogens. Four serotypes. designated A, B, C, and D, are known, with types A and D being responsible for most human disease. Serological differences are due to the number of xylose side chains and degree of O acetylation. The best method used for observing this encapsulated organism is by performing India-ink stain; since ink pigment particles do not have the ability to cross the capsule, a halo if formed around the stained cells (Figure 2; 3). In infected individuals, cerebrospinal fluid is used to identify the presence of this fungus. In addition, cryptococcal antigen testing can also be used to diagnose infection. Figure 2. Cryptococcus neoformans stained with India Ink to show the capsule. Figure 3. India-ink preparation is used primarily to examine cerebral spinal fluid for the presence of the encapsulated yeast Cryptococcus neoformans. This is an India-ink preparation froman exudate containing encapsulated budding yeasts. Virulence and
Pathogenicity: C.
neoformans is able to cause the fungal
infection cryptococcosis due to its
capsule, which enables the yeast to escape
phagocytosis by monocytes or neutrophils, since
Cryptococcal polysaccharide and capsule are
resistant to ingestion. Another virulence factor
is the production of melanin pigments. Melanins
are insoluble polyanionic molecules which
contain stable populations of free Leukocyte adhesion to the endothelium is initiated by the activation of endothelium by cytokines, interleukin-1 (IL-1) and tumor necrosis factor-α, already present at the site infection. This leads to endothelial cytokine production and the upregulation of adhesion molecules. The first step of adhesion is the margination and rolling of leukocytes on the activated endothelium and depends on interactions between selectins (E-selectin on endothelium, P-selectin on platelets and endothelium, and L-selectin on leukocytes) and their counterligands. The leukocytes are then activated by cytokines, which results in the shedding of L-selectin from the leukocyte surface and the increased expression of integrins. The integrins are involved in the subsequent firm binding of the leukocytes to the ligands (the intercellular adhesion molecules (ICAM) and vascular cell adhesion molecule-1) expressed on endothelium, after which the cells finally transmigrate. C. neoformans glucuronoxylomannan interferes with these binding processes, leading to a diminished efflux of leukocytes in the direction of the inflamed tissues (Ellerbroek et al., 2002). Clinical Infections: Many cases of cryptococcosis occur in immunocompromised patients, especially patients with AIDS, suggesting an important contribution of CD4+ cells to immunity. However, cryptococcosis also occurs in pigeon handlers because of the long-term survival of the fungus in pigeon droppings to which the handlers are constantly exposed. The infection is usually acute or chronic, affecting the central nervous system, but may also involve the skin, lungs, urinary tract, eyes, myocardium, and bones. In fact, most infections with C. neoformans consist of a lung infection. However, fungal meningitis, especially as a secondary infection for AIDS patients, is often caused by C. neoformans, making it a particularly dangerous fungus. Infections with this fungus are rare in those with fully functioning immune systems. For this reason, C. neoformans is sometimes referred to as an opportunistic fungus. Treatment: Cryptococcosis that does not affect the central nervous system can be treated with fluconazole alone. Cryptococcal meningitis should be treated for two weeks with intravenous Amphotericin B (0.7 to 1.0 mg/kg/day) and oral flucytosine (100 mg/kg/day) or intravenous flucytosine (75 mg/kg/day) if the patient is unable to swallow. This should then be followed by oral fluconazole 200 mg daily for ten weeks and then 200 mg daily until the patient's CD4+ count is above 100 for three months and, if infected, the host's HIV viral load is undetectable. Treatment with flucytosine does not result in a cure (full clearance of infection and immunity). Rather, it merely suppresses the fungus and does not kill it; viable fungus can continue to be grown from cerebral spinal fluid of patients who have taken fluconazole for many months. An increased dose of 400 mg daily does not improve outcomes either, but preliminary data shows that very high doses of 1200 mg or more per day may be effective. The duration of this treatment and the post-treatment maintenance dose is not known. Furthermore, intravenous Ambisome (4 mg/kg/day) may also be used, but is not superior. Its main use is in patients who do not tolerate Amphotericin B. Those who have HIV, however, must take on a different regime of medicines to treat infection. References: Ellerbroek, P.M., Hoepelman, A.I.M., et al. (2002). Cryptococcal Glucuronoxylomannan Inhibits Adhesion of Neutrophils to Stimulated Endothelium In Vitro by Affecting Both Neutrophils and Endothelial Cells. Infection and Immunity, 70(9): 4762-4771. |